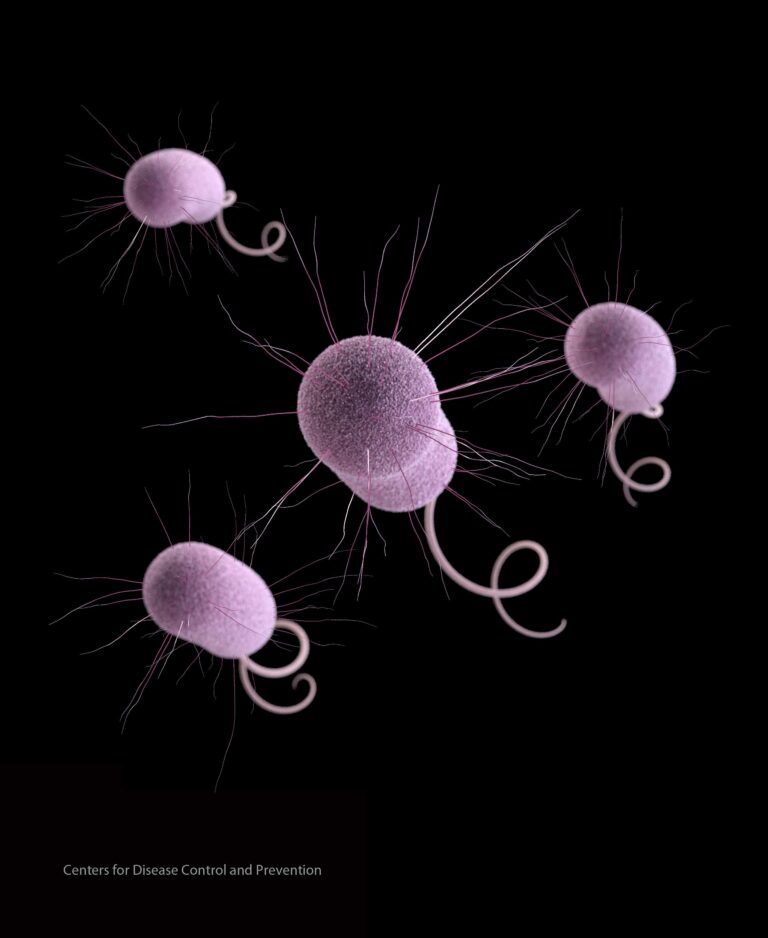
A recent report from the Centers for Disease Control and Prevention (CDC) has raised alarm over a growing public health threat as cases of so-called “nightmare bacteria” continue to rise across the United States. These highly resistant superbugs, known for their ability to evade multiple antibiotics, pose notable challenges to treatment and infection control. The CDC’s findings highlight the urgent need for enhanced surveillance,preventive measures,and new strategies to combat the spread of these dangerous pathogens.
CDC Warns Rising Threat of Antibiotic Resistant Bacteria Across the United States
The latest report from the Centers for Disease Control and Prevention (CDC) highlights a concerning surge in cases caused by antibiotic-resistant bacteria, often referred to as “nightmare bacteria.” These pathogens have evolved mechanisms that negate the effects of conventional antibiotics,rendering some infections nearly impossible to treat. Health officials are especially alarmed by increases in bloodstream infections and pneumonia caused by these resistant strains, which lead to prolonged hospital stays and higher mortality rates.
The CDC identifies several key factors contributing to the rise, including:
- Overuse of antibiotics in both healthcare and agriculture settings
- Slow development of new antimicrobial drugs
- Insufficient infection prevention in hospitals and clinics
- Increased global travel, facilitating the spread of resistant strains
To illustrate the scale of the problem, the agency provides the following overview of antibiotic resistance levels across select bacterial threats:
| Bacteria | Resistance Rate (%) | Annual Cases (Thousands) | Mortality Rate (%) |
|---|---|---|---|
| Carbapenem-resistant Enterobacteriaceae | 60 | 13 | 40 |
| Drug-resistant Neisseria gonorrhoeae | 35 | 550 | 1.2 |
| Multidrug-resistant Pseudomonas aeruginosa | 25 | 32 | 18 |
Factors Driving the Surge in Superbug Infections Revealed in Latest Report
Recent data analysis highlights several key contributors behind the alarming rise in infections caused by multidrug-resistant bacteria, frequently enough referred to as “nightmare bacteria.” Among these, the overuse and misuse of antibiotics in both healthcare and agricultural settings stand out as primary drivers. Widespread prescription of antibiotics for viral infections and the heavy request of antimicrobial agents in livestock have accelerated the evolution of resistant strains, making conventional treatments increasingly ineffective. Additionally, the proliferation of these superbugs is exacerbated by inadequate infection control measures in hospitals and long-term care facilities, where vulnerable patients are most at risk.
Other critical factors include:
- Poor sanitation and hygiene practices across various healthcare environments
- The global movement of people and goods facilitating rapid transmission
- Delayed development of new antibiotics due to economic and regulatory challenges
| Factor | Impact on Resistance |
|---|---|
| Antibiotic Overuse | High |
| Healthcare Hygiene | Moderate |
| Global Travel | Moderate |
| Slow Drug Development | High |
Impact on Healthcare Systems and Patient Outcomes Explored
The rise in cases of antibiotic-resistant “nightmare bacteria” poses a complex challenge for healthcare systems across the nation,straining resources and intensifying the burden on medical professionals. Hospitals are witnessing longer patient stays and increased demand for isolation units to prevent cross-contamination. This surge amplifies costs, sometimes leading to the diversion of critical care resources from other patients. In response, many healthcare facilities are accelerating investments in antimicrobial stewardship programs aimed at optimizing antibiotic use and curbing the spread of resistant infections.
Patient outcomes are equally impacted, with a growing number of individuals facing prolonged illness, higher rates of complications, and increased mortality risk. Vulnerable populations, including the elderly and immunocompromised, are disproportionately affected. The data reveals alarming trends:
- Longer hospital stays: On average, 30% increase in duration compared to non-resistant infections.
- Higher readmission rates: Approximately 25% more frequent within 30 days of discharge.
- Elevated treatment costs: Up to 400% increase due to complex care requirements.
| Impact Metric | Before Rise in Cases | Current Situation |
|---|---|---|
| Average Hospital Stay (days) | 7.2 | 9.4 |
| 30-day Readmission Rate (%) | 12% | 15% |
| Treatment Cost Increase | Baseline | +400% |
Urgent Calls for Enhanced Infection Control and Antibiotic Stewardship Programs
Healthcare facilities across the United States are now facing a critical juncture as the rise of multi-drug resistant bacteria accelerates, challenging the effectiveness of existing infection control measures. Experts emphasize that stringent protocols must be universally adopted to curb the spread of these “nightmare bacteria,” which thrive in hospital environments and compromise patient safety. The CDC underscores the urgency for hospitals to implement complete surveillance systems that promptly identify outbreaks and enforce isolation procedures to prevent cross-contamination.
Key strategies recommended include:
- Enhanced hand hygiene campaigns targeting all healthcare personnel
- Routine environmental cleaning using effective disinfectants
- Regular staff training on infection prevention
- Robust screening for high-risk patients upon admission
Simultaneously occurring, antibiotic stewardship programs (ASPs) are being urged to adopt more aggressive approaches to decrease the inappropriate use of antibiotics—a primary driver behind resistance. These programs must focus on real-time monitoring of antibiotic prescriptions, promoting narrower-spectrum alternatives when possible, and engaging clinicians through feedback and education. A recent CDC analysis highlights noticeable success in facilities that integrated advanced stewardship techniques, translating to measurable reductions in resistant infections.
| Stewardship Intervention | Impact on Resistance | Example Outcome |
|---|---|---|
| Pre-prescription authorization | Decreased needless broad-spectrum use | 30% reduction in carbapenem-resistant infections |
| Audit and feedback | Improved guideline adherence | 20% drop in treatment failures |
| Dose optimization | Minimized toxicity and resistance | Reduced length of hospital stays by 1.5 days |
The Way Forward
As the CDC’s latest report underscores the growing threat of these so-called “nightmare bacteria,” the urgency for enhanced surveillance, robust infection control measures, and accelerated development of new antibiotics becomes ever more apparent. Healthcare providers, policymakers, and the public must remain vigilant in addressing this escalating public health challenge to prevent further spread and safeguard the effectiveness of existing treatments.